The therapeutic use of cannabidiol, better known as CBD, one of the main compounds in cannabis, has gained increasing interest for its beneficial properties on a wide range of medical conditions.
While science is making these discoveries, antibiotic resistance continues to challenge modern medicine, requiring new strategies to combat bacterial infections. Not to mention the countless side effects that antibiotics bring with them.
Against this background, scientists have been asking crucial questions: could CBD make a significant contribution to improving the efficacy of antibiotics? How do CBD’s mechanisms of action intertwine with those of conventional antibiotics? And most importantly, what scientific evidence supports this possible synergy?
In this article, we want to shed light on the relationship between antibiotics and CBD, analysing what science has discovered so far and shedding light on what may be new perspectives in the fight against bacterial infections.
-
Product on sale
 CBD oil 15% (1500mg) Broad SpectrumPrice range: £31.20 through £51.20From 1,71 €/gr
CBD oil 15% (1500mg) Broad SpectrumPrice range: £31.20 through £51.20From 1,71 €/gr -
Product on sale
 CBD oil 25% (2500mg) Broad SpectrumPrice range: £47.20 through £67.20From 2,24 €/gr
CBD oil 25% (2500mg) Broad SpectrumPrice range: £47.20 through £67.20From 2,24 €/gr -
Product on sale
 CBD oil 5% (500mg) Broad SpectrumPrice range: £14.25 through £33.00From 1,10 €/gr
CBD oil 5% (500mg) Broad SpectrumPrice range: £14.25 through £33.00From 1,10 €/gr
Relationship between CBD and antibiotics
As you may already know, CBD has numerous therapeutic properties including an anti-inflammatory effect and the ability to manage anxiety and pain. However, when it comes to combining antibiotics and CBD, it is essential to be very careful and seek prior advice from your doctor.
Antibiotics are powerful drugs used to fight bacterial infections and work in various ways, such as interfering with the bacteria’s cell wall or preventing them from producing essential proteins.
Research suggests that CBD could influence the efficacy of antibiotics, enhancing or decreasing it, depending on the context and the specific drug interaction. For instance, a study from the University of Southern Denmark found that CBD could help fight antibiotic-resistant bacteria, suggesting it as a supporting compound to increase the antibacterial potency of antibiotics.
However, it is important to note that CBD may also interact with the cytochrome P450 system, which is responsible for the metabolism of many drugs, including some antibiotics. This means that CBD could alter the way the body processes antibiotics, potentially leading to an increase or decrease in their levels in the blood.
As we said, however, care must be taken and the individual case must be evaluated. Some antibiotics, such as macrolides, can increase cannabinoid levels in the body, which could lead to an increased risk of adverse effects. Moreover, CBD has been found ineffective against certain types of bacteria, such as Gram-positive bacteria. The interaction of antibiotic and CBD may therefore vary depending on a number of factors.
Antibiotic resistance
As we said at the beginning, antibiotic resistance is a growing global problem that threatens the effectiveness of treatments against bacterial infections. This phenomenon occurs when bacteria mutate or acquire genes whereby they become insensitive to the action of antibiotics, rendering standard treatments less effective or even useless.
Resistance can be intrinsic, i.e. a natural characteristic of the bacterium, or acquired, developing after exposure to an antibiotic. The mechanisms by which bacteria become resistant include modification of the antibiotic’s target site, production of enzymes that degrade the antibiotic, reduction of cell permeability to the antibiotic, and active efflux of the antibiotic out of the bacterial cell.
The misuse and over-consumption of antibiotics, both in human and veterinary medicine, has accelerated the spread of resistance. Self-prescription, the use of antibiotics to promote growth in herds, and inappropriate prescribing by doctors contribute to this problem. In addition, the lack of new antibiotics due to a slowdown in pharmaceutical research and development exacerbates the situation.
Antibiotic resistance not only makes it more difficult to treat infections, but also increases the risk of spreading resistant infections, prolongs the duration of diseases and can lead to increased mortality.
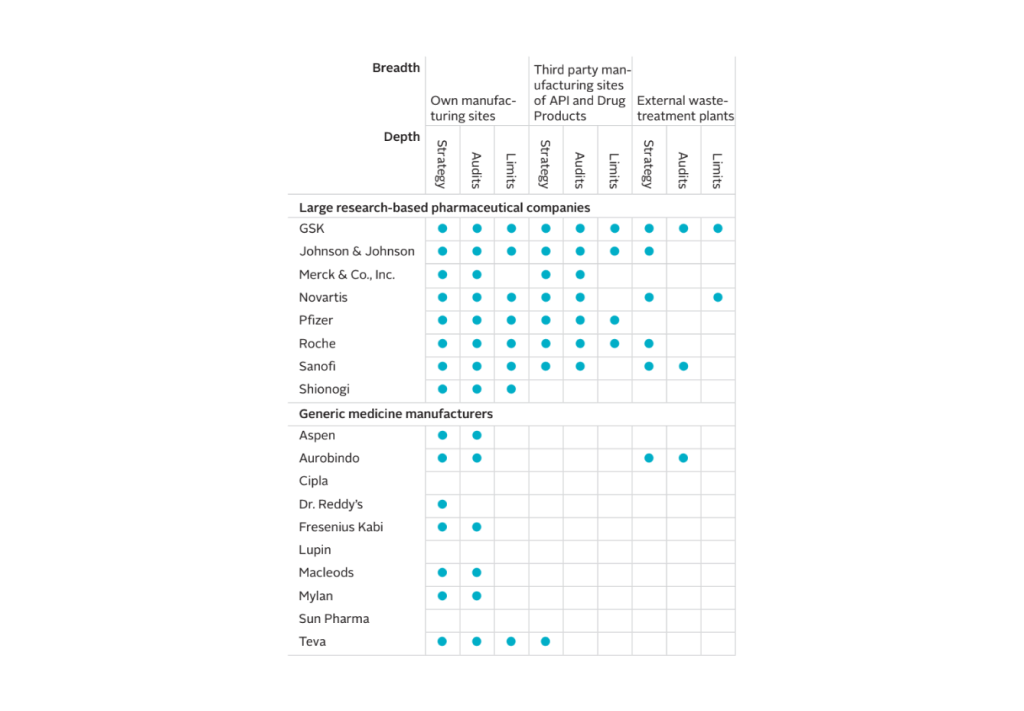
The table shows which pharmaceutical companies have a strategy to minimise the environmental impact of antibiotic waste from production.
Can the effect of antibiotics be improved with CBD?
In the University of Southern Denmark study mentioned earlier, CBD was used to improve the effect of the antibiotic bacitracin against Staphylococcus aureus bacteria, one of the world’s deadliest. During research, the combination of antibiotic and CBD showed a more powerful effect, reducing the amount of antibiotic needed.
In addition to this discovery, which can certainly give hope for treatment methods, the combined use of aid compounds and antibiotics could help to develop fewer resistant bacteria.
Another study showed that CBD can act on the membrane vesicles of Gram-negative bacteria. These vesicles are important for the transport of materials such as proteins, DNA and RNA, and are involved in the communication and attachment processes of bacteria. CBD interacts with these vesicles, enhancing the effect of antibiotics and reducing the amount needed to fight infection.
In addition, CBD has anti-inflammatory properties that may be useful in treating bacterial infections, reducing inflammation and improving the efficacy of antibiotics. This approach could also help reduce the likelihood of bacteria developing resistance to antibiotics, a growing problem in modern medicine.
-
Product on sale
 CBD oil 15% (1500mg) Broad SpectrumPrice range: £31.20 through £51.20From 1,71 €/gr
CBD oil 15% (1500mg) Broad SpectrumPrice range: £31.20 through £51.20From 1,71 €/gr -
Product on sale
 CBD oil 25% (2500mg) Broad SpectrumPrice range: £47.20 through £67.20From 2,24 €/gr
CBD oil 25% (2500mg) Broad SpectrumPrice range: £47.20 through £67.20From 2,24 €/gr -
Product on sale
 CBD oil 5% (500mg) Broad SpectrumPrice range: £14.25 through £33.00From 1,10 €/gr
CBD oil 5% (500mg) Broad SpectrumPrice range: £14.25 through £33.00From 1,10 €/gr
Brief overview of antibiotics
Throughout history, antibiotics have proved to be a key class of drugs in the fight against bacterial infections. These powerful allies of modern medicine are able to kill bacteria or inhibit their growth, allowing the immune system to intervene and resolve the infection. The discovery of antibiotics represented a breakthrough in the treatment of infectious diseases, saving countless lives.
Obviously, the choice of an appropriate antibiotic is crucial to ensure the effectiveness of treatment and minimise the risk of developing antibiotic resistance.
Types of antibiotics
Antibiotics are divided into several classes, each with specific mechanisms of action and spectra of efficacy against various types of bacteria. The main classes of antibiotics include:
- Aminoglycosides;
- Carbapenems;
- Cephalosporins
- Fluoroquinolones
- Glycopeptides and lipoglycopeptides (such as vancomycin)
- Macrolides (such as erythromycin and azithromycin);
- Monobactams (aztreonam);
- Oxazolidinones (such as linezolid and tedizolid);
- Penicillins;
- Polypeptidics;
- Rifamycins;
- Sulphonamides;
- Streptogramins (such as quinupristin and dalfopristin);
- Tetracyclines.
Penicillins, carbapenems, cephalosporins and monobactams are examples of beta-lactam antibiotics, characterised by the presence of a beta-lactam ring in their chemical structure.
The correct use of antibiotics is essential to prevent resistance. This is why it is important to follow the doctor’s instructions regarding dose, frequency and duration of treatment. Stopping antibiotic therapy prematurely or not adhering to prescriptions can not only compromise the effectiveness of treatment but also encourage the development of resistance mentioned above.
How antibiotics work
But how do antibiotics kill bacteria and prevent their growth?
One of the main ways in which antibiotics act is by inhibiting the formation of the bacteria’s cell wall. Antibiotics such as penicillin block the synthesis of this wall, making bacteria unable to resist osmotic pressure, which leads to their destruction.
Some antibiotics, such as sulphonamides, act by mimicking substances that bacteria normally use in their metabolism, such as para-aminobenzoic acid (PABA), which is necessary for the synthesis of folic acid in bacteria. Without folic acid, bacteria cannot produce DNA, RNA and proteins, and therefore cannot grow or reproduce.
Antibiotics can also interfere with protein synthesis in bacteria. For example, aminoglycosides bind to the ribosomal subunits of bacteria, thus blocking the production of essential proteins. This prevents the bacteria from performing vital functions and leads to their death or prevents their reproduction.
Another mechanism by which antibiotics can work is by inhibiting DNA transcription in bacteria. Drugs such as rifamycins interfere with the enzyme RNA polymerase, which is necessary for the synthesis of messenger RNA and, consequently, for DNA replication. This process blocks the life cycle of the bacteria and kills them.
There are also other mechanisms by which antibiotics can exert their action, such as altering the permeability of the cell membrane, inhibiting other essential metabolic pathways or interfering with the synthesis of nucleic acids.
Contraindications of antibiotics
The side effects of antibiotics are an important reality to consider when facing drug treatment for bacterial infections. Although antibiotics are essential to fight infections, they can also cause adverse reactions in the body.
Here is an overview of the most common side effects associated with antibiotic use:
- Gut dysbiosis, which occurs when antibiotics disrupt the natural balance of bacteria in the gut causing symptoms such as diarrhoea, bloating and abdominal cramping;
- Allergic reactions, which can range from mild rashes to more severe conditions such as anaphylactic shock;
- Digestive side effects such as nausea, vomiting and diarrhoea;
- Candidiasis, due to altered microbial flora;
- Alterations in liver or kidney function, as they may affect organ function, such as the liver and kidneys;
- Neurological effects, including dizziness and tinnitus, although these are rare.
For this reason, antibiotics should never be taken lightly or without consulting a doctor.
CBD as support for antibiotics
This fascinating field of study offers promising possibilities for the future of CBD therapy.
If you would like to test the benefits of CBD and integrate it into your wellness routine, we invite you to discover the range of products on the CBD Shop offered by Maria CBD Oil.
With high-quality products and formulations designed to meet individual needs, we are committed to providing reliable and transparent solutions for your health.
Find out now how you can make your body stronger against external attacks.
 Contact us
Contact us 






